History
In the 1950s, birth defects caused by thalidomide1 highlighted the effects environmental-related factors had on fetal development (Brown et al., 2019). Despite evidence of alcohol being apparent from as early as 7,000–6,600 BCE, it wasn’t until 1973 that “fetal alcohol syndrome” was recognised.
The term “fetal alcohol syndrome” (FAS) was first published in 1973 in an article in the British medical journal ‘The Lancet’ by a group of American dysmorphologists, paediatricians and psychiatrists at the University of Washington Medical School.
The article, titled “Pattern of Malformation in Offspring of Chronic Alcoholic Mothers”2, was the first to describe the connection between maternal alcohol abuse and a specific pattern of birth defects. This article provided physicians with the diagnostic criteria for the condition.
Currently, Fetal Alcohol Syndrome (FAS) is categorised within the wider spectrum of Fetal Alcohol Spectrum Disorder (FASD), which encompasses conditions such as Alcohol-Related Neurodevelopmental Disorder, Alcohol-Related Birth Defects, and Neurobehavioral Disorders linked to prenatal alcohol exposure.
Prevalence
It is widely recognised that alcohol can harm the developing fetus, and many recommendations suggest that women avoid drinking alcohol during pregnancy and while nursing. Despite this advice, a significant number of women continue to drink during pregnancy even after discovering they are expecting.
Worldwide, approximately 10% of women in the general population consume alcohol during pregnancy, although the European region has the highest rate of consumption (25%).
A study3 from the National Survey on Drug Use and Health that analysed 2015–2018 data from the reports that:
- About 1 in 10 (9.8%) pregnant women report current alcohol use.
- About 1 in 22 (4.5%) pregnant women report binge drinking.
- Alcohol use is highest among women who are in the first trimester of pregnancy, with about 1 in 5 (19.6%) reporting current alcohol use and 1 in 10 (10.5%) reporting binge drinking.
- About 40% of pregnant women who report current drinking also report current use of one or more other substances—most commonly tobacco and marijuana.
Signs & symptoms
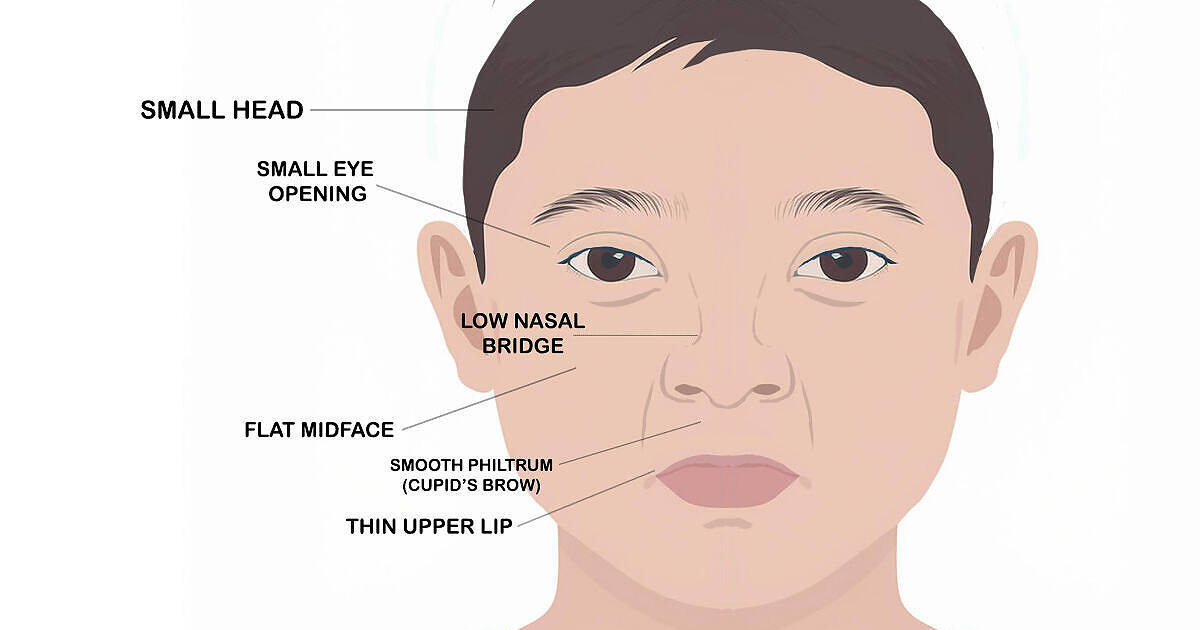
The term fetal alcohol spectrum disorder (FASD) refers to the wide range of physical, behavioural, and cognitive impairments that occur due to alcohol exposure before birth.
Depending on the features identified, the disorders categorized as FASD include:
- Fetal alcohol syndrome
- Partial fetal alcohol syndrome
- Alcohol-related neurodevelopmental disorder
- Alcohol-related birth defects
- A neurobehavioral disorder associated with prenatal alcohol exposure
People with FASD may have difficulty in the following areas:
- Learning and memory
- Understanding and following directions
- Switching attention between tasks
- Controlling emotions and impulsivity
- Communicating and developing social skills
- Experiencing depression and anxiety
- Performing daily life skills, including feeding, bathing, counting money, telling time, and minding personal safety
Prevention
Recognising the underlying factors that lead to alcohol consumption during pregnancy is essential for promoting prenatal health education and reducing the risks of FASD and negative health impacts on both mother and child.
There is no known safe level of alcohol during pregnancy. Recent research published in the journal Alcohol Clinical & Experimental Research4 found that even low to moderate alcohol use by pregnant patients may contribute to subtle changes in their babies’ prenatal development, including lower birth length and a shorter duration of gestation.
This study highlights why it’s essential that pregnant women understand the effects alcohol may have on their babies.
Education
The most commonly reported reasons for alcohol use in pregnancy were societal pressure and the belief that alcohol can be consumed as long as the “strength” and the quantities consumed are low.
Other reasons were a lack of awareness of adverse effects on the fetus; coping with life’s adversities such as depression, domestic violence or poverty; consumption based on intuitive decision‐making and influenced by personal/peer experiences; belief in the beneficial properties of alcohol; advice from medical practitioners; unwanted or unplanned pregnancy; alcohol dependence; and consumption as a cultural/traditional custom.
The best point of pregnancy to educate women about the dangers of fetal alcohol syndrome is at the first prenatal appointment. Usually, patients are asked a series of questions by their midwife, which includes questions on their relationship with alcohol and other drugs.
The temptation to deny alcohol or drug use is expected due to the fear of judgment from healthcare professionals. With this in mind, it would be beneficial for midwives to explain the risks of fetal alcohol syndrome, whether the mother admits to alcohol use or not.
Support
Educating pregnant women at prenatal appointments may be one of the most effective strategies for combating casual alcohol use during pregnancy. If, however, an individual is an alcoholic, seeking addiction support is advisable.
Pregnant women addicted who attend support groups for addiction recovery have a much higher chance of maintaining and achieving long-term addiction recovery. Support groups also offer much-needed emotional support.
Women who abuse alcohol during pregnancy should confide in their prenatal midwife or doctor, who will link them to the relevant addiction services. Attending rehabilitation, addiction counselling, and groups such as Alcoholics Anonymous (AA) and SMART Recovery can be effective for anyone struggling with alcohol addiction.
Unfortunately, the shame carried by pregnant women addicted to alcohol or other drugs can stop them from seeking the help they need. Fear of judgement and worries about being subject to supervision or their child being taken from them prevent women from admitting their alcohol problem during antenatal appointments.
Alcoholism is considered a disease characterised by compulsive drug seeking and use despite adverse consequences. It is considered a brain disorder because it involves functional changes to brain circuits involved in reward, stress, and self-control. Therefore, it seems unjust that society uses stigmatising language to describe pregnant women who abuse alcohol. Not only is it unjust, but it exacerbates the issue because pregnant women are less likely to seek help, which inevitably could leave their child susceptible to the effects of fetal alcohol spectrum disorder.
Sources
-
- Brown, J. M., Bland, R., Jonsson, E., & Greenshaw, A. J. (2019). A brief history of awareness of the link between alcohol and fetal alcohol spectrum disorder. Canadian Journal of Psychiatry, 64(3), 164–168. https://doi.org/10.1177/0706743718777403
- Jones, Kenneth L., David W. Smith, Christy N. Ulleland, and Ann P. Streissguth. “Pattern of Malformations in Offspring of Alcoholic Mothers,” The Lancet 1 (1973):1267–71.
- England LJ, Bennett C, Denny CH, Honein MA, Gilboa SM, Kim SY, Guy GP, Tran EL, Rose CE, Bohm MK, Boyle CA. Alcohol use and co-use of other substances among pregnant females aged 12–44 years — United States, 2015–2018. MMWR Morb Mortal Wkly Rep. 2020;69(31):1009–14. PubMed PMID: 32759915
- Ludmila N. Bakhireva, Xingya Ma, Alexandria Wiesel, Fiona E. Wohrer, Jared DiDomenico, Sandra W. Jacobson, Melissa H. Roberts. Dose–response effect of prenatal alcohol exposure on perinatal outcomes. Alcohol, Clinical and Experimental Research, 2024; DOI: 10.1111/acer.15284





